“Tirzepatide and weight loss surgery”
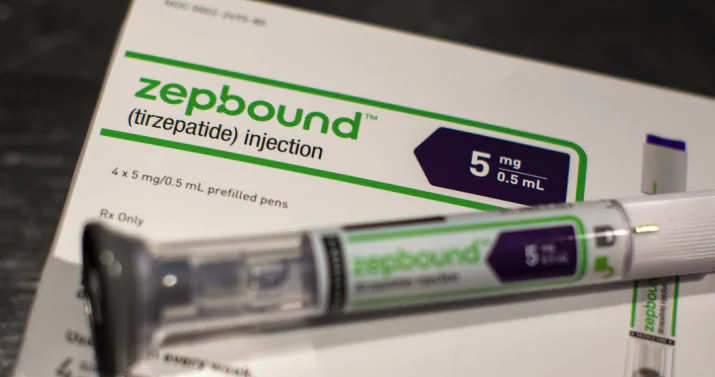
Tirzepatide (known as Mounjaro for diabetes and Zepbound for weight management) and Weight Loss Surgery (Bariatric Surgery) in detail. This is an evolving area in obesity medicine, involving several potential scenarios:
- Defining the Components:
Tirzepatide: An injectable medication, a dual GIP and GLP-1 receptor agonist. It works by mimicking hormones that regulate appetite, insulin secretion, and gastric emptying, leading to improved blood sugar control (for Mounjaro users) and significant weight loss (a key effect for both Mounjaro and Zepbound users).
Weight Loss Surgery (Bariatric Surgery): Includes procedures like Sleeve Gastrectomy, Roux-en-Y Gastric Bypass, Duodenal Switch, etc. These surgeries alter the digestive system (stomach size and/or intestinal path) to restrict food intake and/or reduce nutrient absorption, leading to substantial and often durable weight loss and improvement in obesity-related comorbidities.
- Potential Scenarios & Considerations:
Here’s how Tirzepatide and bariatric surgery might interact:
Scenario A: Tirzepatide Before Bariatric Surgery
Purpose:
Pre-operative Weight Loss: Surgeons or insurance plans often require patients to lose a certain amount of weight before surgery to reduce surgical risks (e.g., decrease liver size, improve anesthesia safety). Tirzepatide’s potent weight loss effect can be a valuable tool to help patients meet these targets.
Improving Comorbidities: Significant weight loss before surgery can improve conditions like type 2 diabetes, hypertension, and sleep apnea, potentially making the patient a better candidate for surgery and improving post-operative outcomes.
“Bridging” to Surgery: Can help patients initiate significant lifestyle changes and experience metabolic improvements while awaiting surgery.
Key Considerations:
Discontinuation Before Surgery: This is crucial. Tirzepatide (like other GLP-1 agonists) delays gastric emptying. This increases the risk of aspiration during anesthesia. Current guidelines generally recommend stopping weekly GLP-1 injections like Tirzepatide at least one week (or sometimes longer, based on anesthesiologist/surgeon preference) before elective surgery requiring anesthesia or deep sedation. Close coordination between the prescribing physician, surgeon, and anesthesiologist is essential.
Not a Replacement (Usually): While significant weight loss might occur, it doesn’t necessarily negate the long-term benefits or anatomical changes provided by surgery for eligible candidates seeking maximum durable weight loss and comorbidity resolution.
Scenario B: Tirzepatide After Bariatric Surgery
Purpose:
Addressing Weight Regain: It’s common for patients to experience some weight regain years after bariatric surgery. Tirzepatide can be considered as a tool to help manage this regain and get back on track.
Suboptimal Weight Loss: For patients who didn’t achieve the expected amount of weight loss after surgery.
Managing Persistent/Recurrent Comorbidities: Particularly for Type 2 Diabetes, which might persist or return even after initial post-surgical remission.
Key Considerations (This scenario requires significant caution and expertise):
Altered Gastrointestinal (GI) Anatomy & Physiology: Bariatric surgery fundamentally
changes the GI tract. This can affect:
Drug Absorption: While Tirzepatide is injected and bypasses first-pass metabolism, altered gut hormone signaling post-surgery might theoretically interact with its mechanism, though this is not fully understood.
Tolerance: Post-bariatric patients often have increased sensitivity to GI issues. The common side effects of Tirzepatide (nausea, vomiting, diarrhea, constipation, abdominal pain) might be more pronounced or harder to tolerate after surgery.
Gastrointestinal Side Effects: Careful, slow dose titration is essential, potentially starting at lower doses or titrating up more slowly than in non-surgical patients. Overlapping symptoms (e.g., nausea from surgery vs. nausea from the drug) can complicate management.
Nutritional Risks: Bariatric surgery inherently carries risks of vitamin and mineral deficiencies due to altered absorption and restricted intake. Tirzepatide’s potent appetite suppression could potentially exacerbate inadequate nutrient intake if not carefully managed with dietary counseling and supplementation monitoring.
Limited Specific Data: While the use of GLP-1 agonists (including Tirzepatide off-label or Zepbound on-label where appropriate) post-bariatrically is increasing, there is still limited large-scale, long-term clinical trial data specifically studying Tirzepatide in this population. Much of the current practice is based on clinical experience, smaller studies, and extrapolation from non-surgical populations or other GLP-1s.
Type of Surgery: Tolerance and effects might differ depending on the type of bariatric surgery performed (e.g., restrictive vs. malabsorptive).
Scenario C: Tirzepatide as an Alternative to Bariatric Surgery
Purpose:
For individuals who meet the criteria for bariatric surgery but prefer a non-surgical approach.
For those who have contraindications or prohibitive risks for surgery.
Key Considerations (Comparison):
Efficacy: Bariatric surgery generally produces higher average long-term weight loss (often 25-35%+ of total body weight) and potentially more durable comorbidity resolution compared to medications alone. However, Tirzepatide (Zepbound) has shown unprecedented weight loss results for a medication (up to ~22% average body weight loss in clinical trials).
Risks: Compare surgical risks (anesthesia, leaks, infections, hernias, long-term nutritional deficiencies, bowel obstructions) versus medication side effects (primarily GI, potential rare risks like pancreatitis or thyroid C-cell tumors noted in animal studies).
Invasiveness & Reversibility: Medication is non-invasive and effects cease upon stopping; surgery involves permanent anatomical changes.
Long-Term Data: More extensive long-term (decades) data exists for bariatric surgery outcomes compared to Tirzepatide.
Cost & Access: Both can be expensive and subject to insurance coverage complexities. Access to qualified surgeons vs. medication availability/coverage varies.
Patient Commitment: Both require significant long-term lifestyle changes (diet, exercise) for optimal success. Medication requires ongoing adherence to injections.
Essential Element: Multidisciplinary Care
Regardless of the scenario, decisions involving Tirzepatide and bariatric surgery require close collaboration and communication between:
The Patient
Bariatric Surgeon
Endocrinologist or Obesity Medicine Specialist (often the prescriber of Tirzepatide)
Primary Care Physician
Registered Dietitian (crucial for nutritional management, especially post-surgery)
Anesthesiologist (if surgery is planned)
Conclusion:
Tirzepatide and bariatric surgery are both powerful tools for managing obesity and related comorbidities. They can potentially be used sequentially (Tirzepatide before surgery for preparation, or after surgery for weight regain/suboptimal loss) or as alternatives to each other. However, combining them or using Tirzepatide in the context of prior surgery requires careful consideration due to altered GI physiology, potential for amplified side effects, nutritional risks, and the current lack of extensive, specific long-term data. Decisions must be highly individualized and made under the guidance of an experienced multidisciplinary healthcare team.

“Tirzepatide and weight loss surgery”
Route
Doctor G Medical Excellence: Health Well-being and Longevity
URL: https://doctorgmed.com/
| Monday | 09:00 - 17:00 |
| Tuesday | 09:00 - 17:00 |
| Wednesday | 09:00 - 17:00 |
| Thursday | 09:00 - 17:00 |
| Friday | 09:00 - 17:00 |
| Saturday | 09:00 - 17:00 |
| Sunday | Closed |